Robert Montgomery walked deliberately down the hospital hallway carrying a stainless-steel bowl containing a living human kidney resting on a bed of ice. Minutes earlier the organ had been in one man's body. It was about to be implanted into another man to keep him alive.
It was about 11 A.M. on a Monday this past spring. I followed Montgomery, an abdominal transplant surgeon and director of the NYU Langone Transplant Institute, into an operating room where 49-year-old John Primavera was waiting to receive the precious kidney. Monitors beeped; Shakira played on the sound system. Montgomery, who has performed thousands of transplants, walked up to the operating table and gently lowered the organ into Primavera's abdomen. The kidney, offered to Primavera by his close friend Thomas Kenny, was pale and about the size and shape of a mango. Montgomery motioned for me to step toward the table. I watched as he removed the clamps on the artery he had just sewn onto the replacement organ. The kidney flushed pink with blood and began to pulse with life.
This kidney transplant was Primavera's second. He was born with a condition called renal hypoplasia, which prevented his own kidneys from fully developing. He had his first transplant at age 14, and that organ lasted about 35 years. But in 2022 it started to fail, and he had to go on dialysis and join the transplant waiting list. Kenny—who has been friends with Primavera since they were in elementary school—voluntarily got tested and found out he was a close tissue match for Primavera. For Kenny, the decision was easy. “I just felt it was the right thing to do at the right time,” he told me a few weeks after the operation.
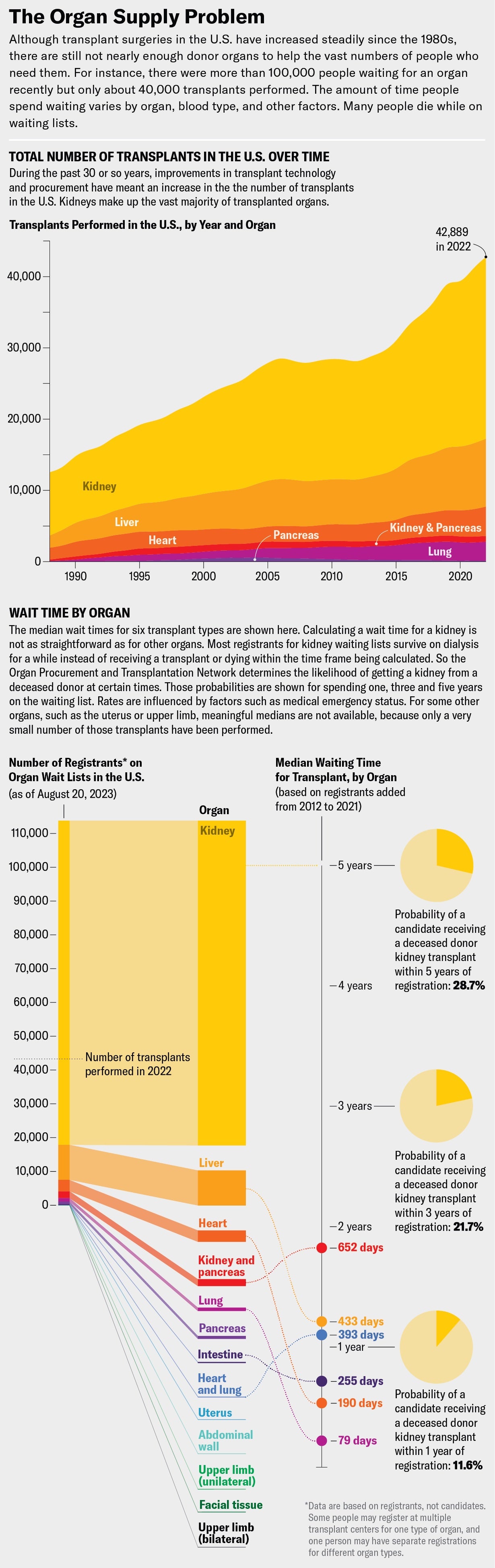
Not everyone is as fortunate as Primavera. More than 100,000 people in the U.S. are currently on waiting lists for an organ transplant, the vast majority of them for kidneys. Every day 17 people die waiting for a transplant. The procurement system uses only a small fraction of the available organs at any particular time because of logistical and medical hurdles and a controversial distribution system. Transplants remain out of reach for too many people, especially those of color and with low incomes; many never even get put on a waiting list.
Recent medical advances in treating infections such as hepatitis C and HIV have made previously unusable organs usable. In addition, technology has made it possible to keep organs viable for longer outside a body before a transplant and even to improve their quality. Yet the demand for organs still far outstrips the supply.
The persistent, tragic situation of people dying on long waiting lists has motivated Montgomery and several other scientists to begin a bold experiment: transplanting organs from other species—specifically, genetically modified pigs—into humans. In the past two years they have made significant progress in these operations, known as xenotransplants. The term has its roots in the Greek word xenos, for “alien” or “foreign.” In tests this year, pig kidneys functioned in human bodies for up to two months without failing. Scientists have figured out genetic tweaks to these organs that make them more compatible with people, reducing the risk of bad reactions or outright rejection by a person's immune system.
[Listen to the Science, Quickly, podcast about the pig kidney transplanted into a human body]
Montgomery compares the current, inadequate organ transplant system to an economy running on fossil fuels. “You can have it burn cleaner, you can make all these various changes,” he says, “but it's still never going to be what you really need, which is something that's renewable, that is sustainable.” Xenotransplants, for Montgomery, are renewable energy.

They are, however, still very much experimental. They present thorny ethical issues such as the questions of who should receive one and how to communicate the risks involved. Some people criticize xenotransplantation as a distraction from addressing the problems with the existing transplant system. But Montgomery strongly disagrees. “I've spent my whole career trying to make these incremental changes,” he says. Now is the time for something bigger, he argues, and xenotransplantation is the answer.
I can relate to the anxiety of waiting for an organ that may never come. My mother was diagnosed in 2019 with pulmonary fibrosis, a progressive and deadly lung-scarring illness with a two- to five-year prognosis, on average, after diagnosis. The disease has no cure, but a lung transplant offered the possibility of extending her life. Like many in need, we had to wait until she was sick enough to be listed for transplant (if she even qualified) while hoping that she would receive an organ before she got too sick to survive the surgery. I know the agony of hoping for a surgical miracle while simultaneously preparing to grieve a parent who is slipping away.
Montgomery also understands this anxiety: he received a heart transplant in 2018 to treat a life-threatening congenital heart condition, which his father and a brother both died from. “My interest in transplant really goes back to when my father was sick,” he told me a few months before Primavera's operation. We were in his office overlooking midtown Manhattan. The walls were decorated with photographs of presidents he had met at ceremonies honoring him or his wife, a mezzo-soprano singer with the Metropolitan Opera. Montgomery's father was diagnosed with dangerous heart disease at age 50, and a heart transplant might have saved him. But at the time, he was considered too old for the surgery. One of Montgomery's brothers died waiting for an organ; another got a transplant and is still alive. When Montgomery became very ill, he had no idea whether he would receive a transplant in time. A heart became available, and Montgomery's own colleagues performed the surgery at NYU Langone Health, where Montgomery currently practices.
Most transplant organs come from deceased donors, but kidneys and parts of other organs, including livers, can be obtained through the generosity of living donors. In the early 2000s, in an effort to increase the supply of organs from living donors, Montgomery performed some of the first “domino”-paired kidney transplants in the U.S., in which multiple donors and recipients provide and receive organs in a kind of surgical daisy chain. The process increases the number of possible matches: if an organ isn't the right blood or tissue type for a donor's intended recipient, it could match someone else in the chain, and another donor in that chain could have an organ that's a good match for the original recipient. Yet such procedures have not markedly increased the number of living-donor kidney transplants, Montgomery says.
The other major source of organs—deceased donors—relies on people who have suffered untimely deaths under circumstances that allow their organs to be retrieved in time for transplantation. These are usually victims of accidents or brain injuries who have been declared brain-dead but whose other organs will keep working as long as the body is kept on life support. Nearly 15,000 deceased people who were registered organ donors or whose families consented on their behalf provided organs in 2022 in the U.S. Historically, a large proportion of deceased donors have been victims of motor vehicle crashes. As traffic and vehicle safety have improved, crashes have become—thankfully—increasingly survivable. Yet the safety improvements have also decreased the number of organs available for transplant.
One development has been driving an increase in donor organs, but it's nothing to celebrate. It's the opioid epidemic. People who die of drug overdoses now constitute a significant fraction of donors—rising from 1 percent of donors in 2000 to more than 13 percent in 2017—and it doesn't seem like the crisis will abate anytime soon. “Our success right now is based on a failure in our society,” Montgomery says. The increase in transplanted organs from people who died from overdoses is a result of the scale of those deaths, as well as of advances in medicine that have made more of those organs usable. Some people who suffer from opioid addiction are also infected with hepatitis C, a disease that causes severe liver inflammation. Until a few years ago, organs from such donors were considered unusable because of the risk of infecting the recipient. But new antiviral drugs have made the disease treatable. Building on work at Johns Hopkins University and the University of Pennsylvania, Montgomery and his colleagues helped to pioneer the first transplants from hepatitis C–positive donors; the heart Montgomery received came from such a donor. And in 2019 surgeons at Johns Hopkins Medicine performed the first kidney transplant in the U.S. between living people with HIV, something that is now done rarely but increasingly often.
These successes notwithstanding, the pool of potential organ recipients has outstripped supply for years. In 2022 more than 42,800 organs, a record number, were transplanted in the U.S.—an increase of 3.7 percent from 2021. With medical care for end-stage organ disease improving, more people are living long enough to make the transplant list, creating demand for more organs.
This unmet need has long disturbed Martine Rothblatt, who has the resources and ambition to do something about it. I first encountered Rothblatt, a biotech entrepreneur and lawyer who founded satellite radio company SiriusXM, at a 2013 conference on futurism and transhumanism, a field focused on enhancing humans using technology. She was giving a talk about her goal of achieving digital immortality by uploading human consciousness to computers. Despite these far-fetched ambitions, Rothblatt has funded a wealth of well-grounded research for decades, and her company United Therapeutics has propelled much of the recent progress in xenotransplantation.
Rothblatt became interested in transplants when her six-year-old daughter was diagnosed with pulmonary arterial hypertension, a lung disease that can be progressive and is sometimes fatal. Doctors told Rothblatt the only treatment was a lung transplant, but the chances of getting one were slim—especially for a child. Rothblatt started a foundation—and later United Therapeutics—to develop drugs for the condition, which have kept her daughter alive. But for many people with this disease, a lung transplant is still the only option, and it became clear to Rothblatt that there simply weren't enough organs to go around. “My near-term plan was that I was going to come up with something to save our daughter Jenesis before she needed a transplant,” Rothblatt says. “My long-term plan was that I would come up with an unlimited supply of transplants.”
Rothblatt and United Therapeutics are pursuing several approaches to achieve this goal. The company is investing in systems that can keep lungs alive outside the body until they are ready to be transplanted. The machines pump oxygen and nutrients through the lungs and keep them warm—a process called ex vivo lung perfusion. Similar systems have been used for years for kidneys and in some cases livers. Only 20 percent of donor lungs are usable because the organs are so susceptible to damage or infection, according to Brandi Zofkie, senior director at Lung Bioengineering, a subsidiary of United Therapeutics. Lung Bioengineering uses a device called XPS, approved by the U.S. Food and Drug Administration and made by the company XVIVO, to perfuse and monitor donor lungs. Donor lungs are sent to Lung Bioengineering's facilities, and its staff conducts real-time video and audio calls with transplant surgeons to evaluate whether a pair of lungs is suitable. “We [try] to remove all the reasons they might say no to an organ,” Zofkie says. The goal, she explains, is to maintain or improve the quality of the lungs prior to transplant by treating any infections and stabilizing their function.
Despite these advances, there are still not enough organs for all who need one. So Montgomery and other scientists have begun to explore a more plentiful source of organs by growing them in animals bred for this purpose.
Xenotransplantation dates at least to the 19th century, when doctors performed skin grafts using frog skin. Other attempts were more bizarre and grotesque: in the 1920s a surgeon in France transplanted chimpanzee testes into elderly men in an attempt to “rejuvenate” the men. More serious attempts happened in the 1960s, when a few intrepid surgeons transplanted kidneys, livers and hearts from chimpanzees and baboons into humans. Some people died soon after the transplants; others survived for months but ultimately experienced infection, rejection or other complications that proved fatal.
In the 1970s and 1980s advances in immunosuppressive drugs made the prospect of transplanting organs from other species more viable. In 1984 an infant known as Baby Fae received a baboon heart and lived for three weeks before her immune system rejected the organ. The surgery generated a lot of publicity around the lack of transplantable infant organs, but it also underscored the immunological challenges of cross-species transplants. After that, the field took a brief pause until the early 1990s. “There was sort of a moratorium on any further xenotransplantation until we were able to develop things further with the advent of some new technologies,” Montgomery says.
There were a few more xenotransplants in the 1990s, but it became clear that better immunosuppression alone would not solve the problem. So scientists began modifying genes that triggered immune reactions. In 2000 PPL Therapeutics (now Revivicor) created the first cloned pigs and began genetically engineering them as a source of organs for human transplants. In 2011 United Therapeutics acquired Revivicor. The company chose pigs in part because the animals are easy to raise but also because their organs are similar to humans' and can be grown to the right size for a human recipient.
[Read more about the monkeys with transplanted pig kidneys living up to two years or more]
In addition, using pigs, which are plentiful and already bred for human use, was considered more ethically acceptable than using nonhuman primates. Revivicor's scientists bred a line of pigs in which they knocked out, or deactivated, the alpha-gal gene, which causes the animals to make a sugar that prompts an immune response in humans. In 2020 the FDA approved these “GalSafe” pigs for use in medical products or as food.
Two years later surgeons at the University of Maryland School of Medicine transplanted a Revivicor pig heart into a man named David Bennett, Sr., making headlines. Bennett had a fatal heart disease and was ineligible for a human heart transplant; he was offered the pig heart under an FDA expanded access protocol (sometimes called a “compassionate use” exception) because his death was otherwise imminent.
The transplanted heart worked for nearly two months before failing. It's not entirely clear why the heart failed; the cause might have been an undetected pig virus, although an analysis the University of Maryland team published in the Lancet suggested that runaway inflammation and reduced immunosuppression might also have played roles. “A surgeon doesn't like to lose a patient,” says Bartley Griffith, Bennett's surgeon. “But it was such a ceiling-breaking event.” Some people have argued that Bennett was too sick to benefit from the transplant, but Griffith says the pig heart was Bennett's best option and that the surgery provided valuable information about how pig organs can work in human bodies. He and his colleagues completed a second pig heart transplant in a man named Lawrence Faucette in September 2023, also under a compassionate use pathway.
In 2021 Montgomery and his colleagues at NYU Langone and transplant surgeon Jayme Locke and her colleagues at the University of Alabama at Birmingham (UAB) separately transplanted pig kidneys into people who had suffered brain death—known as decedents—with the families' consent. These experiments were done to show that pig organs could function in a human body without causing harm.
In the first two NYU surgeries, the kidney was attached to the recipient's upper leg near the groin, where it was more accessible for monitoring, and then connected to the leg arteries and veins. The UAB team transplanted its kidney into the decedent's abdomen. All the transplanted kidneys produced urine—a sign of healthy kidney function. The team ended the experiments after several days, but in that time the organs showed no immediate signs of rejection. In June and July 2022 the NYU group, led by cardiac surgeon Nadar Moazami, transplanted two genetically modified pig hearts into deceased recipients. The transplanted hearts functioned well for the three-day duration of the experiment.
Locke, director of UAB's Comprehensive Transplant Institute, says she got involved in xenotransplantation to help translate the work of basic scientists into a life-extending therapy. “Every week I see a large number of patients that we ultimately wait-list,” she says. “And I know that because of the organ shortage, many of these individuals will die before they ever have the opportunity to receive a transplant. I see xenotransplantation as a way to potentially give hope to many more people.”
In July 2023 NYU invited me to observe its third pig kidney xenotransplant into a human decedent. I watched from the hospital roof as the kidney was delivered by helicopter over New York City's East River. A small team carried a cardboard box holding the organ on ice and pushed it through the hospital hallways in a wheelchair. I followed the team as far as the surgical floor—I couldn't go into the operating room because of the risk of being exposed to a pig virus. Pigs can carry viruses such as porcine cytomegalovirus, the one that was detected in Bennett, the person who received a pig heart transplant in 2022. NYU has developed a more sensitive test for such viruses, but as a precaution, the surgeons and observers receive regular blood tests for them as well.
I watched the transplant via a video feed from the hospital's “control room,” which was packed with doctors and researchers labeling vials that would later contain urine, blood and tissue from both the kidney and the decedent for subsequent analysis.
We waited anxiously as Montgomery and his colleagues connected the pig kidney's blood vessels and ureter to the decedent's. A pig thymus gland—a source of immune cells—was also transplanted to help reduce the risk of immune rejection. As the doctors removed the clamps on the new organ's blood vessels, the kidney started making urine. The graft was working.
After the surgery, Montgomery and his colleagues led a briefing at the decedent's bedside. I took a moment to privately acknowledge the tremendous generosity of the person's family, who, in the midst of immense personal tragedy, made the choice to donate their loved one's body to give someone in the future a better chance at life. The man, named Mo, had died from complications of a brain tumor. His sister, Mary Miller-Duffy, says she made the decision to donate his body because she felt he would have wanted to help people. Kidney disease claimed the life of her other brother when he was just three months old. She told me she struggled with the decision to donate Mo's body, but the compassion of the NYU doctors helped to make it easier. “If I had to do it again, I wouldn't change anything,” she says.

Unlike previous xenotransplants, which were slated to go on for only a few days, this one was planned to last for a month as long as the body and the organ were working without signs of irreversible organ rejection. The procedure went better than expected. At the end of August the experiment was extended for another month. The kidney showed mild signs of rejection, which were reversed before the experiment ended. In August, Locke and her team at UAB reported another kidney xenotransplant into a decedent. That organ was maintained for a week before the experiment was stopped.
Although experiments like these provide useful data, proving that such transplants are safe and effective will require clinical trials in live patients. The FDA has signaled that it is open to starting phase I clinical trials of xenotransplants once it has enough preclinical data. The teams at the University of Maryland, NYU Langone and UAB hope to be among the first the perform them. The prospect of trials in living people raises questions about who gets to participate and how to communicate the risks, says Karen Maschke, a senior research scholar at the Hastings Center who studies the ethics of xenotransplantation. “What kind of eligibility criteria should be in place?” she says. “Because not everybody's going to get access to that first trial.”
Only a very small number of people will be in the first live tests. The researchers leading the trials will have to decide whether to enroll people on transplant waiting lists or people who are not eligible for human organ transplants and thus have no other option, Maschke says. Participants will probably also end up being people who live near the transplant centers doing the trials, for logistical reasons.
Although human welfare is the biggest concern, xenotransplants also bring up questions about the ethics of raising animals for their organs. Animal welfare groups have asked whether it is ethical to kill an animal to save a human life. Xenotransplant advocates counter that animals raised to feed people vastly outnumber any that would be used for transplants. The latter are likely to be strictly regulated by the FDA because their organs would be considered drugs, Maschke notes. The biggest hurdle may be a more existential one—the idea of putting pig organs into humans may disturb some people. Yet history shows that medical procedures once considered unnatural can become routine. Pig heart valves and cow heart tissue are now widely used in medicine, for instance.
Ambitious plans are in the works to produce more organs. Montgomery and other researchers are working on ways to take animal organs, strip away their cells and seed them with stem cells from a human recipient so the person's body won't reject the transplant. The NYU team plans to implant such “decellularized” organs in a recently deceased person sometime soon, Montgomery says. United Therapeutics is working on making 3-D-printed organs out of cells and tissues that could be customized to any person. And other research is changing the definition of death itself: researchers at Yale University have developed a perfusion system for keeping pig brain cells and bodies “alive” for hours after the animals have died. One day this system might be able to preserve human organs for transplantation or even revive people on the brink of death.
Even as scientists expand the boundaries of transplant science, however, there is enormous room for improvement in the current system. Surgeons frequently pass up good organs because they lack the staff and other resources to use them. Since the 1970s the United Network for Organ Sharing (UNOS) has been the sole entity responsible for matching organ donors and recipients in the U.S. It works with several dozen nonprofit groups contracted by the Department of Health and Human Services to get organs from donors to hospitals. But flaws in this system, such as lack of accountability and outdated software, have limited its effectiveness. In March the Biden administration announced plans to modernize the transplant system by making it more competitive, and in July the U.S. Congress passed legislation to break up UNOS's monopoly.
My mom made the transplant list in the fall of 2021. On December 15 of that year, she got “the call”: a pair of lungs was available that might be a match for her, and could she please come to the hospital as soon as possible to get checked in for transplant surgery? Qualifying for the transplant list was an arduous process that took close to a year. It involved lots of testing, with many possible disqualifiers, and all the while my mom's health continued to deteriorate. After she made the list and spent several months on it, we endured an agonizing day of waiting in the hospital while the surgeon made sure the lungs were of suitable quality. (Too often they are not, and the patient is sent home.) The lungs were deemed good, and my mom was wheeled into the operating room. Seven hours later she was wheeled out with a new chance to live.
My mom has marked a year and a half with her new lungs. Recovery wasn't easy—she experienced a lot of pain in her rib cage, which her surgeons had to cut apart to put in the organs, and she had a brief lymphoma scare. The transplant recuperation process took a heavy emotional toll on my siblings and me, who spent nearly two months caring for her. But she has since recovered well.
With her gift of health and time, she has now moved back to Hawaii, where she lived for many years before her transplant. Among the first things she did after her return were to paddle in a Hawaiian outrigger canoe with her old canoe club and to swim in the Pacific Ocean without an oxygen tank for the first time in years. I have immense gratitude for her donor and their family, for the expert medical team that performed the surgery and cared for her afterward, and for the generations of medical advances that came before. Thanks to them, I still have my mom.


